Vital pulp therapy
Vital Pulp Therapy (VPT): Comprehensive Overview and Clinical Protocol
1. Introduction and definition
Vital Pulp Therapy (VPT) encompasses a set of clinical procedures aimed at preserving the vitality of the entire pulp or part of it when compromised by caries, trauma, or iatrogenic exposure. Unlike conventional root canal treatment, which relies on complete pulp removal and chemo-mechanical preparation of the root canal system, VPT is based on the biological principle of pulp healing and regeneration and respects minimal invasiveness. Thus, the pulp retains its natural functions – defense, immunity, sensation, and regeneration.
⸻
2. Historical background and current position
• 1756 – Pfaff: first description of covering exposed pulp with gold foil.
• 1921 – Datweiler: first clinical comparison of materials (best results with ZOE – zinc oxide eugenol cement).
• 1920–1930 – Hermann: introduction of Ca(OH)₂, which became the standard for decades.
• 1990s – Torabinejad: introduction of MTA, a breakthrough in sealing ability, biocompatibility, and stimulation of hard tissue formation.
• Today: widespread use of calcium silicate cements (MTA, Biodentine, bioceramic putties) – improved handling, shorter setting time, color stability (ZrO₂ replacing Bi₂O₃).
Originally, VPT was mainly indicated in children and adolescents with teeth presenting an open apex (where apexogenesis was the main goal). Thanks to bioactive materials and a deeper understanding of pulp biology, indications have now expanded to include adults with closed apices, provided vital tissue remains and correct protocols are followed.
VPT is now regarded as a predictable alternative to root canal therapy, often with comparable – and in carefully selected cases, even better – outcomes.
⸻
3. Biological basis and healing process
When the irritant is removed and a hermetically sealed, clean environment is established, the following biological processes occur:
• suppression of the inflammatory response,
• activation of mesenchymal stem cells from the pulp (and from the apical papilla in younger patients),
• differentiation of odontoblast-like cells producing reparative dentin,
• stabilization and long-term survival of the vital tissue.
The success of VPT depends on preserving a sufficient portion of healthy pulp capable of mounting a biological response, along with strict infection and bleeding control.
⸻
4. Indications
• Reversible pulpitis (symptomatic/asymptomatic) – short-lasting pain after stimulus, subsiding upon removal.
• Traumatic pulp exposure (crown fracture, luxation/avulsion with intact blood supply).
• Iatrogenic pulp exposure during cavity preparation.
• Carious pulp exposure without signs of irreversible involvement (no spontaneous pain, no purulent exudate).
• Children and adolescents – teeth with an open apex (pulp vitality essential for root development).
• Adults – teeth with a closed apex, provided part of the pulp complex remains healthy.
⸻
5. Contraindications
• Clinical signs of irreversible pulpitis (spontaneous/prolonged/nocturnal pain, persistent pain after thermal stimulus, purulent exudate). Still, the boundaries of indications are shifting, and in some cases with these symptoms, VPT may still be worth attempting if vital tissue remains and hemostasis can be achieved.
• Pulp necrosis.
• Significant periapical pathology (large radiolucency, pathological resorption, fistula).
• Inability to achieve reliable rubber dam isolation.
• Patient unwilling to cooperate or attend follow-up visits.
⸻
6. Diagnosis
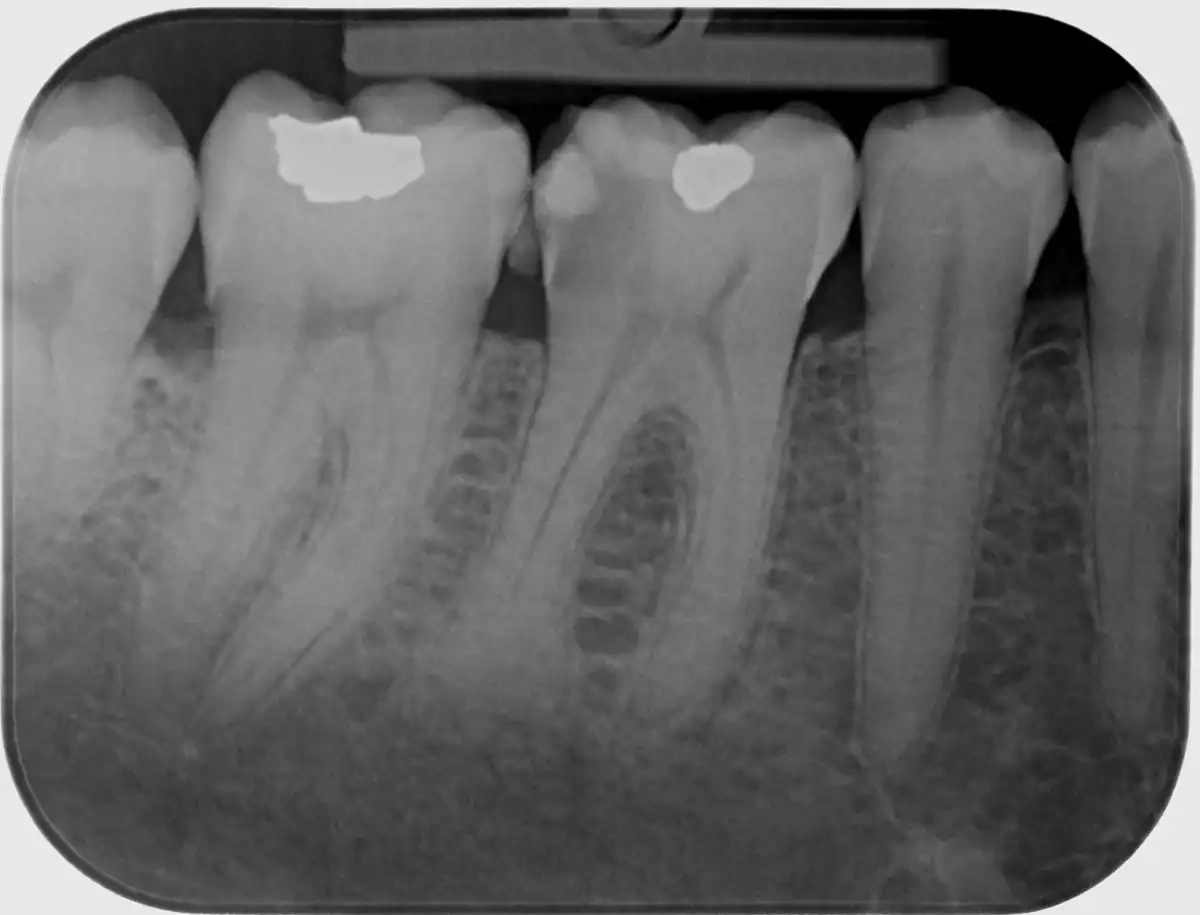
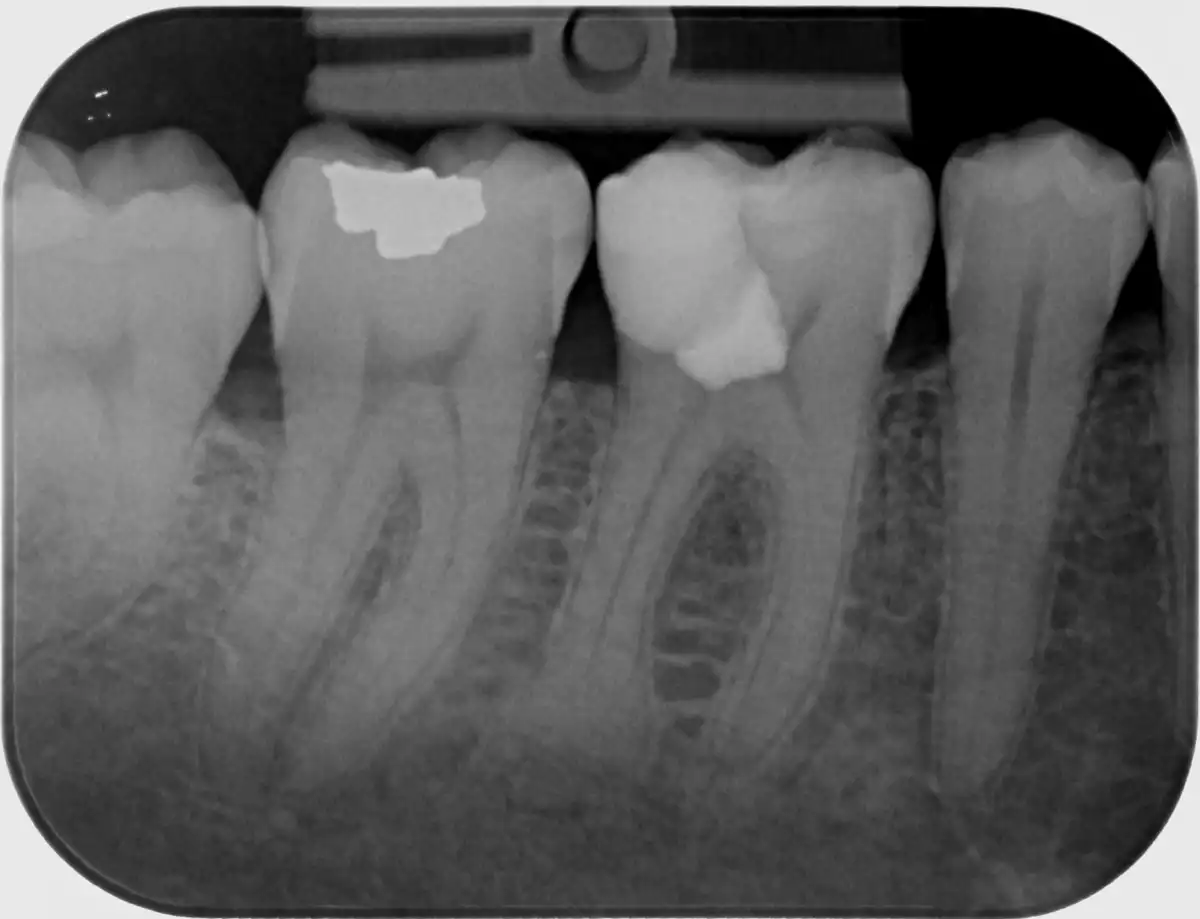
• Clinical examination: absence of spontaneous/nocturnal pain, positive response to vitality tests; time required to achieve hemostasis is a key prognostic factor (ideally within 2–5 minutes).
• Radiographic examination: periapical radiograph or CBCT, absence of apical osteolysis; evaluation of residual tooth structure, root morphology, and factors influencing coronal seal quality.
⸻
7. Clinical protocol (step by step)
1. Anesthesia and isolation: local anesthesia, absolute isolation with rubber dam.
2. Caries removal and preparation: conservative but complete caries removal at the periphery (DEJ); in deep lesions, selective removal in the deepest area to prevent exposure.
3. Exposure and pulp assessment: under magnification (loupes/microscope), evaluate pulp color, bleeding characteristics, necrotic foci, and signs of hyperemia.
4. Hemostasis and disinfection: sterile cotton pellets with 3–6% NaOCl, applied for 2–5 minutes until clean hemostasis is achieved; repeat as needed, followed by sterile saline rinse.
5. Choice of VPT type:
• Direct pulp capping – small, clean exposure with rapid hemostasis,
• Partial pulpotomy – removal of 1–3 mm of coronal pulp in deeper exposures or presence of dentin shavings,
• Full pulpotomy – removal of the entire coronal pulp while preserving vital radicular pulp.
6. Placement of bioactive material: calcium silicate cement (MTA, Biodentine, bioceramic putty), 1–2 mm layer over the pulp.
7. Base/liner: if indicated, cover with a thin layer of glass ionomer.
8. Definitive restoration: ideally immediate adhesive composite restoration with strict coronal sealing; in children, provisional GIC may be used with later definitive buildup.
⸻
8. Materials
Materials of choice:
• MTA (Mineral Trioxide Aggregate),
• Biodentine,
• other modern calcium silicate-based materials with similar biological properties.
Characteristics: alkaline pH, antibacterial effect, high biocompatibility, stimulation of hard tissue formation, sealing ability, and color stability in newer generations.
⸻
9. Possible complications
• Persistent or worsening pain → treatment failure, requiring root canal therapy.
• Internal resorption (rare; usually due to misdiagnosis or incorrect indication).
• Tooth discoloration (with some MTA formulations).
• Microleakage if coronal seal is inadequate.
⸻
10. Prognosis and follow-up
With proper indication and meticulous performance, VPT achieves success rates above 90%. Key factors: accurate diagnosis, controlled hemostasis, use of bioactive cements, and a hermetic coronal seal.
Follow-up: clinical and radiographic evaluations at 6, 12, and 24 months.
⸻
11. Importance of magnification
Working under a dental microscope (or at least loupes) increases diagnostic certainty and treatment quality. It allows detection of subtle differences in pulp tissue (hyperemia vs. necrosis), accurate bleeding assessment, and controlled application of materials. These factors directly improve prognosis.
⸻
12. Borderline indications
The boundary between reversible and irreversible pulpitis is not absolute. Clinical experience shows that VPT can be successful even in borderline cases if vital tissue remains and hemostasis is achieved.
Even in the presence of a periapical lesion, VPT may be considered if pulp vitality is clinically confirmed and bleeding is controlled – outcomes can be favorable.
⸻
13. Practical tips
• 5×3 rule: planning the extent of excavation reduces the risk of accidental exposure.
• Caries-detecting dyes refine the excavation endpoint; the peripheral zone must be caries-free.
• IDS + resin coating and allowing the hybrid layer to stabilize for 5 minutes (so-called time “decoupling”) improve sealing quality.
• If calcium silicate does not set as expected, place a temporary closure and delay definitive restoration – priority is biology and sealing.
⸻
14. Perspectives of calcium silicate materials
• Current: MTA – biocompatible but long setting time and risk of discoloration; Biodentine – faster setting, color stable; bioceramic putties – excellent handling, sealing ability, color stability.
• Future:
1. Even faster and more reliable setting for true single-visit treatments.
2. Permanent color stability, including in the anterior region.
3. Enhanced bioactivity (Ca²⁺/Si release) with predictable dentin bridge formation.
4. Hybrid systems (Ca-silicate × resin) combining biological activity with improved sealing.
5. Standardization of hemostasis protocols (NaOCl: concentration/time) to unify clinical practice.
⸻
15. Conclusion
Vital pulp therapy is today a clinically established and scientifically supported biologically conservative strategy. When properly indicated and performed, it reliably preserves pulp vitality and long-term tooth function.
Key pillars of success: strict isolation, bleeding control, use of calcium silicate cements, hermetic coronal seal, and work under magnification.
Another advantage of VPT is that it avoids complications of root canal treatment – perforations, fractured instruments, inadequate disinfection, or long-term failures. These complications can occur even in the hands of experienced endodontists.
The historical journey from gold foil through Ca(OH)₂ to modern bioceramics highlights a clear trend: preserve vitality whenever biologically and technically possible.